By Dr Tee E Siong
Consultant Nutritionist and Chairman, Positive Healthy Ageing Programme Malaysia

Introduction
Osteoporosis, also known as “porous bone disease”, is a bone condition where bone mineral density and bone mass decreases, therefore making bones more fragile and susceptible to fractures. This is commonly seen during ageing, but the reality is that bone mass begins to decline as early as our mid-30’s. Malaysians are at a higher risk of osteoporosis with the prevalence of a staggering 24.1% among post-menopausal women, therefore underlining the importance of understanding this condition.

Osteoporosis – A disease that can often go unnoticed
A distinctive feature of osteoporosis is its “silent” nature, which refers to the way the disease manifests in
individuals. At first, individuals may not experience any noticeable symptoms when they start to lose bone
mass. However, as the condition progresses, individuals may experience symptoms such as persistent back pain and a loss of height over time. In addition, estimates indicate that 33.3% of women aged over 50 years and 20% of men will experience an osteoporosis-related fracture, particularly in the wrists, hips and spine. In fact, osteoporosis related fractures are recognised as a major health problem by the World Health Organisation (WHO).

Osteoporosis and risk factors
The risk factors of osteoporosis can be divided into two categories: non-modifiable and modifiable factors.
Non-modifiable factors include things we cannot change, like getting older, having a family history of hip
fractures, having a personal history of fractures, ethnicity, or gender. Interesting, these latter two have been shown to have a significant impact on osteoporosis. In fact, older women who have undergone menopause are particularly vulnerable. Looking at the local study in Malaysia, it was found that Chinese individuals had the highest rates of hip fractures compared to Malays and Indians. Notably, the study highlighted that Chinese women faced a significant risk, accounting for 44.8% of all hip fractures.
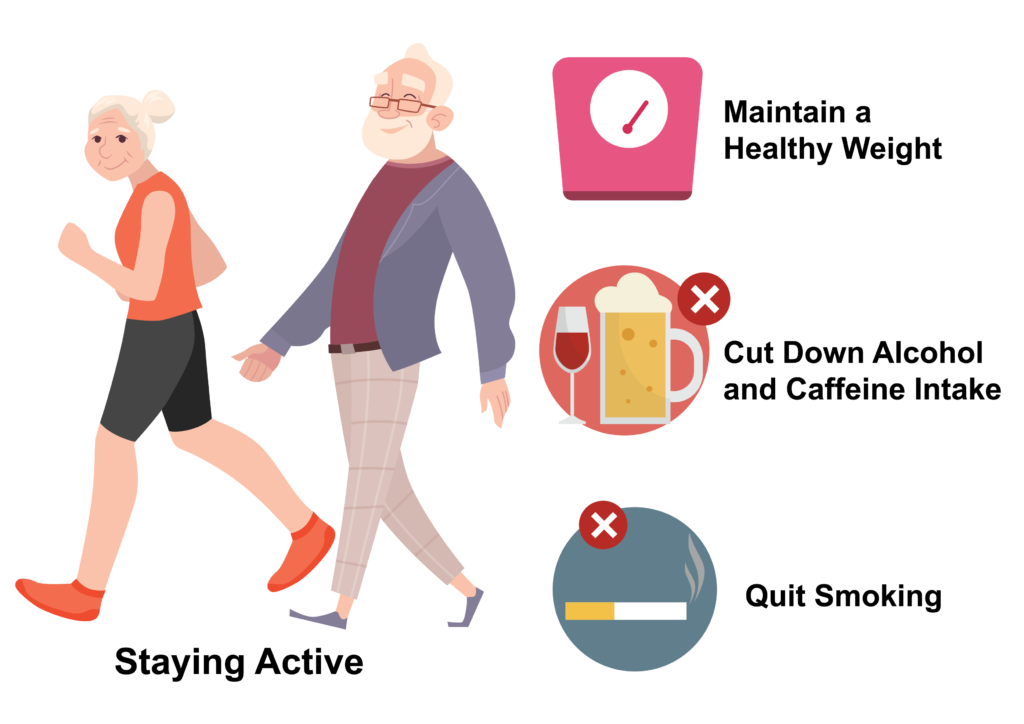
On the other hand, modifiable factors include things that we can changes, for example our calcium or vitamin D intake, our lifestyle, smoking habits, and alcohol and caffeine intake.
Taking steps to prevent osteoporosis
To keep your bones strong to prevent osteoporosis, it is important to consider making changes in your
nutritional intake, physical activity and to regularly attend health screenings.
Preventing osteoporosis through nutrition and active living
Preventing osteoporosis is important, and it’s never too late to take the right steps, even if you’re ageing. One of the most important things you can do is to eat right. This involves eating a balanced, varied, and moderate diet in order to provide your body with the necessary nutrients to build and maintain strong bones. One helpful guideline is to follow the Malaysian Healthy Plate (“Suku-Suku-Separuh”), which suggests dividing your meal into quarters: one-quarter for protein-based foods, one-quarter for carbohydrate-based foods, and half for fruits and vegetables. This approach makes it easier to ensure you’re getting the right nutrients to support your bone health.
In addition to following the Malaysian Healthy Plate concept, it is important to include foods that are rich in bone-protecting nutrients i.e. calcium and vitamin D. Calcium is important to keep the bone healthy and prevent osteoporosis while vitamin D helps the body absorb calcium better. Good sources of calcium-rich foods include milk, yoghurt, cheese, green leafy vegetables such as broccoli and kailan, tofu, sardines and beans; while vitamin D can be found in foods such as salmon, sardines, canned tuna, egg yolk, cereals and dairy products fortified with vitamin D. Alternatively, one can simply boost vitamin D production by spending 10-15 minutes in the sunlight each day.

Leading a healthy lifestyle is also vital. Staying active by walking, jogging, or climbing stairs is important, as is keeping a healthy weight. Include muscle strengthening exercises such as tai chi or sit-to-stand exercise in daily physical activity is important too as these can help to strengthen the muscles which are important for supporting healthy bones. Additionally, as we age, it is advisable to cut down on alcohol and caffeine intake and to quit smoking if you are a smoker. These habits will not only help protect your bones but also improve your overall health and well-being, to help you stay mobile and maintain independence for living a healthy life.
Preventing osteoporosis by regularly attending health screenings
Some may not notice any problems with their bones until a minor accident occurs or if they break a bone. Do include screening for osteoporosis as part of your routine health screening. This is especially crucial for those “at-risk” populations, which include women aged 50 years or older and those who have a history of bone fractures, height loss, or regular falls.
It is recommended to speak with a doctor about the tests available for osteoporosis. One such test is the Bone Mineral Density (BMD) test, which measures how strong one’s bones are, predicts the risk of fractures, and helps diagnose osteoporosis. In addition to this, the test can also be used to monitor how well osteoporosis treatments are working. In generally, women aged 65 or older and men aged 70 or older should consider having a BMD test as part of their regular health screenings.
Conclusion
The skeletal system serves as the fundamental framework of our body, providing essential support, enabling movement, and safeguarding vital organs like the heart and brain from harm. It also functions as a “storehouse” for essential minerals. Therefore, we should all take the right proactive measures to ensure our bone health. By doing so, we not only ensure a future with resilient bones but also a life lived well in good health. Remember, healthy bones are the foundation of a stronger you!
This educational article by Positive Healthy Ageing Programme (PHAP) is supported by an educational grant from Anlene Malaysia.